Your cart is currently empty!
Blog
Dr Ashkar
Bonnie has been doing this process for six months so far, as of Sunday, April 9, 2017 19:45:14.
[svpVideo v=1]
[svpVideo v=2]
I do not agree with him that it does not matter if you eat contaminated foods (pesticides, etc) – he says just use his method to remove the toxins.
Dale
His book http://cancerselfcure.com
Distilled Water is Credited for Good Health
Spring 1998, Vol. 30, No. 1
“New Glory to Its Already Gallant Record”
The First Marine Battalion in the Spanish-American War, Part 2By Trevor K. Plante
On reporting that he had dispatched marines to their new duty stations, Huntington concluded his report by stating, “I believe this encampment has been of great benefit to the health of the battalion.”55 The adjutant and inspector of the Marine Corps also found the men at Camp Heywood in good health. In his inspection report the adjutant concluded, “It is worthy of note that during the entire service of this battalion of 25 commissioned officers and 623 enlisted men, from April 22, when they embarked on board their transport at New York to the present time, there has not been a single case of yellow fever nor death from disease of any kind and but few cases of serious illness; a remarkable fact, when it is considered that these men were the first United States troops to land in Cuba, and during their entire service they were subject to the same climatic influences as other troops, among whom fever, diarrhea, dysentery, etc., caused so many casualties.”56
The quartermaster of the battalion reported to the commandant that because of the use of distilled water for drinking and cooking and the sanitary conditions aided by sufficient food and clothing, 98 percent of the battalion was brought home fit for duty, and “not a single man of the command died from disease.”57 The men had used only distilled water obtained daily from the Panther, Resolute, or Vulcan. McCawley also had had the foresight to purchase empty wine casks in Key West for use as water containers, increasing the amount of water that could be kept on hand at camp. The excellent health of the battalion can be attributed to this careful preparation of water.
On September 18 a parade was held in the streets of Portsmouth.58 After the battalion was disbanded, detachments headed for New York, Philadelphia, Norfolk, Washington, and Annapolis left Portsmouth together and passed through the city of Boston. The Washington detachment consisted of 3 officers and 164 men who arrived in Washington on September 22. That morning President McKinley informed the commandant of the Marine Corps that he wanted to review the detachment. Remnants of the battalion were led by the U.S. Marine Band from the Marine Barracks in Washington, D.C. The parade proceeded despite heavy rains while President McKinley and several officers reviewed the troops.59
Individual honors were bestowed upon Sergeant Quick and Assistant Surgeon Gibbs. Sgt. John Quick was awarded the Medal of Honor for “cool and gallant conduct” in signaling the Dolphin on June 14, 1898, at Cuzco, Cuba.60 The secretary of war honored John Gibbs, the assistant surgeon killed at Guantanamo, four months after his death by naming an army hospital in Lexington, Kentucky, after him.61
Although the majority of marines during the Spanish-American War served aboard ship fulfilling various duties from ship guards to gunners mates, the First Marine Battalion received such wide newspaper attention that it dominated the public view of the marines’ role in the war. They received favorable press coverage not only because they were among the first to see action, but because they always encountered an enemy that had superior numbers. The battalion enhanced the reputation of the Marine Corps and showed the American public their usefulness as an American fighting force. Newspapers also reported on the low rate of disease and sickness in the battalion as opposed to the high rate found in army units.
The Spanish-American War showed the navy that the Marine Corps had a role in their future war plans. With the postwar acquisitions of the Philippines and Guam, the navy was now responsible for actively operating in the Pacific Ocean. The navy would need advanced bases and coaling stations if their ships were to successfully operate in this area. The marines would play a vital role, for these bases and coaling stations would need to be captured and held if necessary.62
During the Spanish-American War, the First Marine Battalion demonstrated the fast mobilization of the Marine Corps. The battalion was prepared and displayed something future marines would take pride in— the ability to be called and respond at a moment’s notice. Marine Corps historian Alan Millett observed that for this era the First Marine Battalion “made the greatest contribution to the Marine Corps’s reputation for combat valor and readiness.”63 The battalion could be proud of its accomplishments. The unit dominated what was seen as the Marine Corps role in the war. In his general order acknowledging the one-hundredth anniversary of the Marine Corps in 1898, the secretary of the navy proclaimed that in the war with Spain the Marine Corps added “new glory to its already gallant record.”64
“New Glory to Its Already Gallant Record,” Part 1
Notes
1 Sgt. John Henry Quick received the Medal of Honor on June 14, 1898. Capt. George F. Elliott rose quickly through the ranks and went on to become the tenth commandant of the Marine Corps serving from October 3, 1903, to November 30, 1910. First Lt. Wendell C. Neville went on to serve as commandant of the Marine Corps from March 5, 1929, to July 8, 1930.
2 “Casualties Occurring on the U.S.S. Maine,” Statistical Report, Special Appendix, Bureau of Medicine and Surgery, Annual Reports of the Navy Department for the Year 1898: Report of the Secretary of the Navy. Miscellaneous Reports (1898), p. 793 (hereinafter cited as Navy Dept. Annual Report, 1898).
3 Appendix to Report of Chief of Bureau of Navigation, 1898 (1898), pp. 17 – 18.
4 Huntington served under Maj. John G. Reynolds as a platoon leader at First Bull Run on July 21, 1861. See entry 196, Records of the Bureau of Naval Personnel, Record Group 24, National Archives and Records Administration, Washington, DC (hereinafter, records in the National Archives will be cited as RG ___, NARA); Bernard C. Nalty, The United States Marines in the War with Spain (rev. 1967), p. 7.
5 “Report of the Commandant of United States Marine Corps,” Charles Heywood, colonel commandant, to the secretary of the navy, Sept. 24, 1898, Navy Dept. Annual Report, 1898, p. 822 (hereinafter cited as Commandant’s Report).
6 Commandant of the Marine Corps to the secretary of the navy, April 23, 1898, letter #73, book 7, box 2, entry 6, Press Copies of Letters, Endorsements, and Annual Reports to the Secretary of the Navy, Feb. 1884 – Jan. 1904, Records of the US Marine Corps, RG 127, NARA.
7 Commandant’s Report, p. 823, and Charles L. McCawley to the quartermaster, US Marine Corps, Sept. 27, 1898, Navy Dept. Annual Report, 1898, p. 884.
8 Entry for April 22, “Journal of the Marine Battalion Under LT COL Robert W. Huntington, Apr. – Sept. 1898,” p. 2, entry 153, RG 127, NARA (hereinafter cited as Huntington Journal).
9 John H. Clifford, History of The First Battalion of US Marines (1930), pp. 9 – 10, box 15, Cochrane Collection (PC# 1), Marine Corps Historical Center (MCHC), Washington, DC. Note: The Panther was purchased as the Venezuela on April 19, 1898, from Red D. Line S.S. Co. See Vessels Purchased, Bureau of Construction and Repair, Navy Dept. Annual Report, 1898, p. 516. McCawley to quartermaster, Sept. 27, 1898, Navy Dept. Annual Report, 1898, p. 885.
10 Battalion Order No. 8, USS Panther, entry for Apr. 24, Huntington Journal, p. 53; Clifford, History of the First Battalion, p. 11.
11 Chief of Bureau of Navigation to colonel commandant, Apr. 22, 1898, April 1898 folder, box 46, Historical Division Letters Received, 1818 – 1915, entry 42, RG 127, NARA.
12 Commandant’s Report, Navy Dept. Annual Report, 1898, p. 824.
13 McCawley to commandant, Jan. 8, 1900, Jan. – June 1900 file, and Huntington to commandant, Nov. 3, 1899, July – Dec. File, box 48, entry 42, RG 127, NARA.
14 Commandant’s Report, Navy Dept. Annual Report, 1898, p. 824; entry for Apr. 26, Huntington Journal, p. 2.
15 Pvt. Edward A. Donahue, Company E, was sent to the US Army Hospital in Key West after fracturing his arm from falling off of a Jacob’s ladder, hitting the boat, and falling overboard. See entry for Apr. 29, Huntington Journal, p. 3.
16 Telegram #33, box 1, North Atlantic Station— Naval Base, Key West, Telegrams Recvd May 7 – Aug. 15, 1898, Records of Naval Operating Forces, RG 313, NARA.
17 McCawley to the quartermaster, Sept. 27, 1898, Navy Dept. Annual Report, 1898, pp. 885 – 887.
18 Battalion Order No. 13, USS Panther, entry for Apr. 28, Huntington Journal, p. 58.
19 Entries for May 12, 13, and 15, Huntington Journal, pp. 5 – 6; Clifford, History of the First Battalion, p. 12.
20 Telegram #107, box 1, North Atlantic Station— Naval Base, Key West, Telegrams Recvd May 7 – Aug 15, 1898, RG 313, NARA.
21 Charles L. McCawley, “The Marines at Guantanamo,” (ms., n.d.), p. 11, Folder 2, McCawley Papers (PC #360), MCHC.
22 Entry for June 10, Journal, p. 8.
23 “Extracts from the Autobiography of Admiral B.H. McCalla,” pp. 1 – 2, box 381, OH (Shore Operations), Subject File, Naval Records Collection of the Office of Naval Records and Library, RG 45, NARA; First Indorsement by B. H. McCalla, June 19, 1898, of Colonel Huntington’s report of June 17, 1898, Navy Dept. Annual Report, 1898, p. 839.
24 Entry for June 10, Huntington Journal, p. 8; McCawley, “Marines at Guantanamo,” pp. 12 – 13; McCalla Report No. 85, June 11, 1898, June 11 – 12 folder, box 29, Area 8 File, RG 45, NARA.
25 Clifford, History of the First Battalion, p. 12; Huntington to Heywood, June 17, 1898, Navy Dept. Annual Report, 1898, p. 838; McCawley, “Marines at Guantanamo,” p. 13.
26 Chief signal officer, War Department, to the secretary of the navy, June 11, 1898, and McCalla Report No. 86, June 12, 1898, June 11 – 12 folder, box 29, Area 8 File, RG 45, NARA; McCalla, “Marines at Guantanamo,” p. 11.
27 Huntington to Heywood, June 17, 1898, Navy Dept. Annual Report, 1898, pp. 838 – 839.
28 McCalla, “Marines at Guantanamo,” p. 5.
29 McCawley to Huntington, June 10, 1902, and Huntington to McCawley, June 14, 1902, 1898— June Folder, box 47, entry 42, RG 127, NARA. These two letters identify Lieutenant Draper as raising the first flag over Camp McCalla.
30 James McGolgan and William Dumphy, entry for June 11, Huntington Journal, p. 9; Huntington to Heywood, June 17, 1898, Navy Dept. Annual Report, 1898, pp. 838 – 839. Note: In several sources Dumphy’s name appears as Dunphy.
31 Clifford, History of the First Battalion, p. 13; “Engagements at Guantanamo, Cuba, Marine Battalion, North Atlantic Fleet, June 11 to 20, 1898,” Bureau of Medicine and Surgery, Navy Dept. Annual Report, 1898, p. 798; Spanish-American War volume, entry 36A, Medical Certificates and Casualty Lists, 1828 – 1939, Records of the Bureau of Medicine and Surgery, RG 52, NARA. On June 12 McCalla states in report no. 86 that two privates and one sergeant were killed and that their bodies were mutilated.
32 Commandant’s Report, p. 824, and Huntington to Heywood, June 17, 1898, Navy Dept. Annual Report, 1898, pp. 838 – 839.
33 John R. Spears, Our Navy in the War with Spain (1898), pp. 265 – 266; Clifford, History of the First Battalion, p. 15.
34 Huntington to Heywood, June 17, 1898, Navy Dept. Annual Report, 1898, pp. 838 – 839; Clifford, History of the First Battalion, p. 15; McCawley, “Marines at Guantanamo,” p. 28; “First American Fortifications in Cuba, Playa del Este, Guantanamo Bay, July 9,” The New York Times Illustrated Magazine, July 21, 1898, p. 4, clippings file, box 2, Huntington Collection, PC #276, MCHC.
35 Chaplain’s letter of Aug. 29, 1898, from USS Texas, copied into Huntington Journal, pp. 294 – 296; Spears, Our Navy in the War with Spain, p. 267. Chaplain Jones returned to his launch accompanied by two reporters, George Coffin of the Journal and T. M. Dieuaide of the New York Sun. An account was published in the New York Evening Sun on July 18.
36 McCalla to commanding officer of Panther, June 12, 1898, Marblehead, box 3, North Atlantic Station, Correspondence with Commanders of Vessels, Dec. 1897 – Dec. 1899, RG 313, NARA.
37 Commandant’s Report, p. 824, and Huntington to Heywood, June 17, 1898, Navy Dept. Annual Report, 1898, pp. 838 – 839.
38 Elliott to Huntington, June 15, 1898, ibid., p. 845.
39 McCalla to Sampson, June 16, 1898, p. 846, and Huntington to Heywood, June 17, 1898, ibid., pp. 838 – 839.
40 McCalla to Sampson, June 16, 1898, ibid., p. 846.
41 First Indorsement by McCalla of Elliott’s Report of June 18, 1898, ibid., p. 845.
42 Squadron Bulletin No. 4, Thursday, June 16, 1898, and Squadron Bulletin No. 8, Monday, June 20, 1989, box 461, OO, Subject File, RG 45, NARA; Spears, Our Navy in the War with Spain, pp. 270 – 271; McCalla, “Marines at Guantanamo,” p. 13.
43 McCalla to Huntington, June 18, 1898, Marblehead, box 3, North Atlantic Station, Correspondence with Commanders of Vessels, Dec. 1897 – Dec. 1899, RG 313, NARA.
44 Entry for June 20, Huntington Journal, p. 17; Sampson to Comdr. George C. Reiter, June 21, 1898, 1898— June 20 – 21 folder, Area 8 File, RG 45, NARA.
45 Entry for June 24, Huntington Journal, p. 18. Almost a year later the bodies were disinterred and buried in the United States. On April 29, 1899, the remains were buried in the following locations: Dumphy and Good buried at Naval Cemetery, New York; McColgan buried at Stoneham, Mass.; Smith buried in Smallwood, Md.; and Taurman buried at Richmond, Va. See 1898— April folder, box 46, entry 42, Historical Division Letters Received, 1818 – 1915, RG 127, NARA.
46 Entry for June 25, Huntington Journal, p. 18; Squadron Bulletin No. 13, Saturday, June 25, 1898, box 461, OO, Subject File, RG 45, NARA. On June 28 William F. Arnold, US Navy, joined the battalion as P. Asst. Surgeon; see p. 278, June, 1898 Muster Rolls, RG 127, NARA.
47 Memos (three of July 4 and one of July 5) from New York to McCalla, Marblehead, and memo for Chief of Staff from McCalla, July 7, 1898, box 3, North Atlantic Station, Correspondence with Commanders of Vessels, Dec. 1897 – Dec. 1899, RG 313, NARA.
48 General Order from McCalla, July 12, 1898, Marblehead, box 3, North Atlantic Station, Correspondence with Commanders of Vessels, Dec. 1897 – Dec. 1899, RG 313, NARA; entries for July 23, 26 – 27, Huntington Journal, pp. 23 – 24.
49 Pages 24 – 25, July, 1898 Muster Rolls, RG 127, NARA.
50 Clifford, History of the First Battalion, p. 24.
51 Entries for Aug. 5 and Aug. 9, Huntington Journal, pp. 25 – 26.
52 Goodrich to McCalla, Aug. 13, 1898, Navy Dept. Annual Report, pp. 842 – 843.
53 Entries for Aug. 18 – 19, Huntington Journal pp. 28 – 29; Correspondence Relating to Cuba, April 15 to September 1, 1898, vol. 1, Correspondence Relating to the War with Spain (1902), pp. 234 and 240.
54 Commandant’s Report, Navy Dept. Annual Report, 1898, p. 825; Huntington was promoted to colonel, Elliott advanced three numbers, Lucas to brevet captain, Neville to brevet captain, Magill to first lieutenant and brevet captain, and Bannon to brevet first lieutenant. See Huntington Journal, entry for Aug. 29, p. 28; entry for Aug. 30, copy of letter received from the commandant, pp. 31 – 32; and entry for Sept. 19, p. 33. Order dated Sept. 17, 1898, Order Book No. 40, pp. 898 – 900, box 13, Letters and Telegrams Sent to Officers Conveying Orders (“Order Books”), entry 24, RG 127, NARA.
55 Huntington to commandant, Sept. 21, 1898, 1898 – September folder, box 47, entry 42, RG 127, NARA.
56 “Report of Inspection of the Marine Battalion at Camp Heywood, Seaveys Island, Portsmouth, N.H., September 14, 1898,” Maj. George C. Reid, Sept. 18, 1898, Navy Dept. Annual Report, p. 849.
57 McCawley to quartermaster, Sept. 27, 1898, ibid., pp. 884 – 888.
58 Clifford, History of the First Battalion, p. 26.
59 Commandant’s Report, Navy Dept. Annual Report, 1898, pp. 825 – 826.
60 General Order 504, Navy Department, acting secretary, Dec. 13, 1898.
61 Special Order No. 254, US Army Adjutant-General, Oct. 27, 1898, Extract, Appendix to Report of Chief of Bureau of Navigation, 1898, pp. 441 – 442.
62 Alan R. Millett, Semper Fidelis: The History of the United States Marine Corps (1991), pp. 134 – 135; Jack Shulimson, “Marines in the Spanish American War,” in Crucible of Empire, ed. James C. Bradford (1993), pp. 150 – 151; Nalty, United States Marines in the War with Spain, p. 17.
63 Millett, Semper Fidelis, p. 131.
64 General Order No. 494, Secretary of the Navy John D. Long, July 30, 1898, Commandant’s Report, Navy Dept. Annual Report, 1898, p. 834.
Trevor K. Plante is an archivist in the Old Military and Civil Records unit, National Archives and Records Administration. He specializes in military records prior to World War II.
Bulking Agents – Psyllium Husks – Avoid Taking Near Meals or Vitamins
Common sense reminder about Colon Pills and all bulking items:
Bulking items contain soluble and insoluble fiber. The insoluble fiber sweeps debris through the digestive track.
Here is the caution: It is best to avoid taking nutritional supplements with the bulking items because some of the nutrition may be carried through your digestive system without being absorbed.
We recommend separating the ingestion of the bulking items and meals (or supplements) by 1 1/2 hours.
Diazepam (Valium, Diastat) – Side Effects
[svpVideo v=1]
In the news:
Drug that steals women’s lives: It’s more addictive than heroin, with horrifying side-effects. So why, 50 years after its launch, is Valium still given to millions?
Read more: http://www.dailymail.co.uk/femail/article-2289311/Valium-Its-addictive-heroin-horrifying-effects-given-millions.html#ixzz4dEdqgVxF
Follow us: @MailOnline on Twitter | DailyMail on FacebookWhat are the possible side effects of Diazepam?
Medicines and their possible side effects can affect individual people in different ways. The following are some of the side effects that are known to be associated with this medicine. Just because a side effect is stated here does not mean that all people using this medicine will experience that or any side effect.
Drowsiness, including drowsiness and lightheadedness the next day.
See warnings above.
- Confusion.
- Shaky movements and unsteady walk (ataxia).
- Loss of memory (amnesia).
- Muscle weakness.
- Tremor.
- Dizziness.
- Headache.
- Slurred speech.
- Skin rashes.
- Disturbances of the gut such as diarrhea, constipation, nausea, vomiting or abdominal pain.
- Slow, shallow breathing.
- Paradoxical effects such as restlessness, agitation, irritability, aggression.
- Difficulty passing urine (urinary retention).
- Urinary incontinence.
- Visual disturbances such as blurred vision.
- Changes in sex drive.
- Low blood pressure (hypotension).
- Blood disorders.
- Jaundice.
Talk to your doctor, nurse or pharmacist if you want any more information about the possible side effects of this medicine. If you think you have experienced a side effect, did you know you can report this using the yellow card website?
How can I stop diazepam (Valium)?
Furthermore, “rebound symptoms” can occur, which may manifest in high levels of anxiety. However, these symptoms should begin to decline about 6-8 weeks after quitting Valium. 24 – 72 hours Valium withdrawal: Withdrawal from Valium mimics that of alcohol. Your body will experience tremors, sweating, and agitation
What is Diazepam used for?
Short-term (two to four weeks only) treatment of severe anxiety that is disabling or subjecting the individual to unacceptable distress.
Short-term (two to four weeks only) treatment of severe insomnia that is disabling or subjecting the individual to extreme distress (oral forms of diazepam only).
Relieving anxiety and causing sedation before surgery or medical procedures (pre-med).
Managing symptoms of withdrawal from alcohol (used in combination with other treatment for alcoholism).
Controlling convulsions (fits) caused by poisoning (intravenous and rectal forms of diazepam only).
Controlling repeated fitting with no recovery of conciousness between seizures (status epilepticus) (intravenous and rectal forms of diazepam only).
Controlling fitting associated with fever (febrile convulsions).
Controlling muscle spasms, for example due to tetanus or poisoning.
How does Diazepam work?
Diazepam is a type of medicine called a benzodiazepine. Benzodiazepines are used for their sedative, anxiety-relieving and muscle-relaxing effects.
Diazepam works by acting on receptors in the brain called GABA receptors. This causes the release of a neurotransmitter called GABA in the brain.
Neurotransmitters are chemicals that are stored in nerve cells in the brain and nervous system. They are involved in transmitting messages between the nerve cells. GABA is a neurotransmitter that acts as a natural ‘nerve-calming’ agent. It helps keep the nerve activity in the brain in balance, and is involved in inducing sleepiness, reducing anxiety and relaxing muscles.
As diazepam increases the activity of GABA in the brain, it increases its calming effect and results in sleepiness, a decrease in anxiety and relaxation of muscles.Diazepam has several uses. Firstly, it can be used to calm severe anxiety and agitation. For example, benzodiazepines such as diazepam are effective at quickly reducing the symptoms of anxiety and agitation that occur in a manic episode of the psychiatric illness, bipolar affective disorder. A benzodiazepine may be given as part of the initial treatment of a manic episode, though they are not licensed specifically for this purpose. Benzodiazepines help calm the individual while the main medicines for this condition (mood stabilizers) begin to take effect.
Oral forms of diazepam are also used for short-term treatment of severe anxiety associated with insomnia. Diazepam decreases the time taken to fall asleep and wakings during the night, as well as increasing the total amount of time spent sleeping. However, it is only suitable for short-term treatment of insomnia and anxiety as it has a high potential for dependence and addiction. As diazepam remains active in the body for many hours, drowsiness may also last into the next day.
Diazepam is also given for its sedating and anxiety-relieving effects as a pre-med before surgery or medical investigations and procedures, and to alcoholics during acute alcohol withdrawal (‘cold-turkey’).
The second main use of diazepam is in controlling convulsions, for example, associated with poisoning, or seizures associated with fever in children (febrile convulsions). It is particularly useful for controlling repeated epileptic fits when the person doesn’t recover consciousness between fits (status epilepticus). Diazepam helps control convulsions because the increased activity of GABA that it causes in the brain helps to calm the excessive electrical nerve activity that is responsible for causing seizures.
A further use of diazepam is in controlling muscle spasms due to tetanus or poisoning.
Related Article
Treatments for anxietyHow do I take Diazepam?
Diazepam may be taken as tablets or syrup, or given by injection or rectal solution (enema), depending on what condition is being treated and how fast a response is needed.
Diazepam tablets and syrup can be taken either with or without food.
Always take the medicine as directed by your doctor. Do not exceed the dose prescribed by your doctor.
Things you should know before taking Diazepam?
This medicine causes drowsiness and muscle weakness and impairs concentration and alertness. These effects may continue into the following day and are made worse by drinking alcohol. If you are affected you should not drive or operate machinery.Do not drink alcohol while taking this medicine.
From March 2015 a new ‘drug driving’ law comes into force, which makes it an offence to drive with certain drugs or prescription medicines above specified limits in your body. The list includes diazepam, which means it may be an offence to drive while you are taking this medicine. The new law will allow police to use roadside drug tests to check for the presence of the prohibited drugs in a driver’s saliva. There are very low limits for illegal drugs, but higher limits for prescribed medicines. This should mean that most people taking diazepam as prescribed will not be breaking the law, provided they are not driving dangerously. If you are found to be above the limit for diazepam there is a medical defence if you are taking the medicine as prescribed, as long as your driving is not impaired. If you are taking a high dose of diazepam it may therefore be sensible to carry your prescription with you when driving, in case you are asked to take a test by the police. However, if you are driving dangerously while taking this medicine you will be breaking the law. You should not drive if you think this medicine affects your ability to drive safely, for example if it makes you feel sleepy, dizzy, unable to concentrate or make decisions, or if you have blurred or double vision.This medicine is generally only suitable for short-term use. If it is used for long periods or in high doses, tolerance to and physical and psychological dependence upon the medicine may develop, and withdrawal symptoms may occur if treatment is stopped suddenly.
Treatment with this medicine should usually be stopped gradually, following the instructions given by your doctor, in order to avoid withdrawal symptoms such as rebound insomnia or anxiety, confusion, sweating, tremor, loss of appetite, irritability or convulsions.Children.
Elderly people.
Weak or debilitated people.
Decreased kidney function.
Decreased liver function.
People with disease affecting the airways or lungs (respiratory disease).
People with a history of alcoholism or drug abuse.
People with personality disorders.
Depression.
It is important to tell your doctor if you have recently suffered a loss or bereavement, for example the death of a close friend or relative, before taking this medicine. Benzodiazepines such as this one can affect the way you adjust psychologically to events like this.
Who should not take Diazepam?
People who are allergic to other benzodiazepines.
People with a sudden worsening of any underlying lung disease (acute pulmonary insufficiency).
People with slow, shallow breathing (respiratory depression).
People who suffer from sleep apnoea syndrome, which is a problem involving short spells when breathing stops during sleep.
People with abnormal muscle weakness due to the condition myasthenia gravis.
Long-term psychotic illness.
Phobias or obsessional states.
People who are very restless or hyperactive.
Severely decreased liver function.
Breastfeeding.
This medicine should not be used if you are allergic to one or any of its ingredients. Please inform your doctor or pharmacist if you have previously experienced such an allergy.If you feel you have experienced an allergic reaction, stop using this medicine and inform your doctor or pharmacist immediately.
Can I take Diazepam while pregnant or breastfeeding?
Certain medicines should not be used during pregnancy or breastfeeding. However, other medicines may be safely used in pregnancy or breastfeeding providing the benefits to the mother outweigh the risks to the unborn baby. Always inform your doctor if you are pregnant or planning a pregnancy, before using any medicine.
This medicine may be harmful to a developing baby and it should be avoided during pregnancy unless considered essential by your doctor. This is particularly important during the first and third trimesters of pregnancy and before or during labour. Regular use during pregnancy should especially be avoided, as the baby could become dependent on the medicine and then suffer withdrawal symptoms after the birth. If this medicine is used in late pregnancy or during labour it may cause floppiness, low body temperature and breathing or feeding difficulties in the baby after birth. Ask your doctor for further information.
Significant amounts of this medicine may pass into breast milk. It should not be used by breastfeeding mothers as it may be harmful to the nursing infant. Seek medical advice from your doctor.Related Article
Over-the-counter medicines in pregnancy
ADVERTISEMENT – CONTINUE READING BELOWCan I use other medicines with Diazepam?
It is important to tell your doctor or pharmacist what medicines you are already taking, including those bought without a prescription and herbal medicines, before you start treatment with this medicine. Similarly, check with your doctor or pharmacist before taking any new medicines while taking this one, to make sure that the combination is safe.
Related Article
Is it dangerous to take different medicines at the same time?
There may be an increased risk of drowsiness and sedation if diazepam is taken with any of the following (which can also cause drowsiness):alcohol
antipsychotics, eg chlorpromazine, clozapine
antipsychotics, eg chlorpromazine, clozapine
baclofen
baclofen
barbiturates, eg phenobarbital
barbiturates, eg phenobarbital
other benzodiazepines, eg temazepam
other benzodiazepines, eg temazepam
lofexidine
lofexidine
MAOI antidepressants, eg phenelzineMAOI antidepressants, eg phenelzine
nabilone
nabilone
sedating antihistamines, eg chlorphenamine
sedating antihistamines, eg chlorphenamine
sleeping tablets, eg zopiclone
sleeping tablets, eg zopiclone
strong opioid painkillers, eg morphine, codeine, dihydrocodeine
tizanidine
tricyclic antidepressants, eg amitriptyline.
The following medicines may prevent the breakdown of diazepam in the body. As this could increase the blood level of diazepam and its sedative effects, as well as the risk of its side effects, your doctor may need to prescribe you a lower than normal dose of diazepam if you are taking any of these medicines:cimetidine
disulfiram
esomeprazole
fluconazole
fluoxetine
fluvoxamine
fosamprenavir
isoniazid
itraconazole
ketoconazole
modafinil
oestrogens and progestogens, for example in contraceptives like the pill
omeprazole
ritonavir (diazepam should preferably not be used in people taking ritonavir)
valproatevoriconazole.
Diazepam may enhance the blood pressure lowering effect of medicines that lower blood pressure, particularly medicines used to treat high blood pressure (antihypertensives), diuretic medicines and nitrates for angina. This may cause dizziness, which can usually be relieved by lying down until the symptoms pass.
The following medicines may decrease the blood level of diazepam. As this could make it less effective, your doctor may need to prescribe you a larger than normal dose of diazepam if you are taking any of these medicines:
phenytoin
rifampicin.
Caffeine and theophylline may reduce the sedative and anxiety-reducing effects of diazepam.Diazepam may reduce the effectiveness of levodopa in treating Parkinson’s disease.
Diazepam may increase or decrease blood levels of the anticonvulsant medicine phenytoin.
People who break free from benzodiazepine addictions tend to feel a lot better: Studies show that quitting leads to improvements in cognitive performance, mood and sleeping, and since the prolonged use of a benzodiazepine often causes as many anxiety problems as it’s supposed to solve, quitting generally makes very good sense.
But though quitting is sensible, it’s certainly not easy,especially if you don’t start with a reasonable understanding of the process and a solid plan for success.
So read on to learn more about…
- The nature of benzodiazepine withdrawal symptoms (when they arise, why you get them, what they feel like, how long they last, etc.)
- Why a dangerous cold turkey detox makes no sense at all
- Different tapering methods and schedules (including how and why you might want to switch to long-acting diazepam)
- How to cope with withdrawal symptoms (self-help, medications, counseling etc.)
Benzodiazepine Withdrawal Symptoms
Not everyone quitting benzos will experience withdrawal symptoms and most people experience only a few, not the complete list of possible symptoms.
Typical withdrawal symptoms include:1
- Sleeping problems
- Feeling anxious or tense
- Panic
- Depression
- Confusion
- Paranoia – thinking other people want to do you harm
- Feelings of disassociation
- Abnormal sensory perception (noises sound loud, colors seem odd, etc.)
- Shaking, or more rarely, convulsions
- Muscle aches, pains and spasms
- Irritability
- Symptoms that mimic flu
See the end of this article for a comprehensive list of less commonly experienced withdrawal symptoms.
Why Do You Get Withdrawal Symptoms?
All benzodiazepines work by increasing the activity of the neurotransmitter GABA. Since GABA is an inhibitory transmitter, which slows or stops the firing of other neurotransmitters, by increasing GABA activity you quiet the brain’s overall activity level. GABA is the brain’s natural sedative, and benzodiazepines simply enhance its functioning.
GABA suppresses excitatory neurotransmitters like dopamine, serotonin, epinephrine (noradrenaline) and acetylcholine. These excitatory transmitters play important roles in memory, muscle movement, alertness, emotional regulation, heart rate and blood pressure and hormonal secretions. When taking benzodiazepines you quiet your whole brain’s activity level. This reduces anxiety and insomnia, but also causes changes to many of the body’s essential systems. This is why taking chronic high doses of benzos can cause such a variety of health problems and why people experience such a wide array of withdrawal symptoms after stopping.
Benzodizepine users quickly develop a tolerance and start needing increasingly larger doses to achieve any desired effects. Because of this, most prescribing guidelines advise against the use of benzos for more than 3 or 4 consecutive weeks.
With tolerance:
- The GABA and benzodiazepine receptors compensate for the medication’s continual presence by becoming less responsive to the medication (so less GABA)
- The excitatory systems that are naturally controlled by GABA also adapt by becoming less responsive to GABA inhibition (So less GABA and the GABA that’s left doesn’t do as much)
So once you’ve developed a tolerance you need large doses of benzos to just get the GABA system functioning at a ‘normal’ level. If a person with a benzo tolerance suddenly stops taking their medication, GABA activity drops substantially and this causes equally substantial increases in the activity of the brain’s excitatory dopamine, serotonin, noradrenalin etc. systems.2
In some cases, as your tolerance rises, you can start to experience withdrawal symptoms on a steady dose, and you need to up your daily dosage to keep these withdrawal symptoms at bay.
Do All Benzo Users Get Withdrawal Symptoms?
According to the benzodiazepine dependency advocacy group Reconnexion, between 50% and 80% of people who use benzos for 6 months or longer will experience at least some withdrawal symptoms after stoppage.
The duration of withdrawal symptoms can also vary a great deal, but people who have longer histories of use are more likely to experience longer withdrawal periods than people with shorter use histories.3
You are more likely to have difficult withdrawal symptoms when quitting:4
- After a very long period of use
- When trying to come off a very high daily dosage
- When you have been using potent, fast acting benzodiazepines
When Do Withdrawal Symptoms Start to Occur?
You will start to feel withdrawal symptoms sooner if using a shorter acting benzo, like Xanax, and later, if using a long acting benzo, like valium.
- Users of short acting benzos may start to experience withdrawal symptoms within 2 days of the last dose
- Users of longer acting benzos may start to experience withdrawal symptoms between 2 and 10 days of the last dose5
Withdrawal symptoms may persist for a few days or weeks. Some people experience withdrawal symptoms that persist for months or even years after cessation of use.
How to Quit? Taper Down or Cold Turkey?
Taper. Without a doubt.
If you have been using benzodiazepines on a daily basis for more than three weeks, you should not stop using suddenly – you need to taper down instead.
- A cold turkey detox can be dangerous, or even deadly, and it increases the odds of an agonizing and lengthy withdrawal.
- A slow taper maximizes safety and minimizes discomfort.
You may have an impulse to try to power through quickly and tough it out. Although this is understandable – it’s a very bad idea.
Tapering Methods
Tapering should be slow and gradual (months, not weeks) – it doesn’t really matter how long it takes (it probably took you a long time to build up your tolerance) and what’s most important is making steady progress towards your goal while minimizing your discomfort along the way (see below for example tapering schedules).
By tapering you can
- Minimize your withdrawal symptoms – by reducing at a rate that’s comfortable to you
- Stay in control – you decide how fast you want to go forward and you don’t have to endure strong withdrawal symptoms if you don’t want to
You can do:
- A direct taper – where you make steady reductions off whatever benzo you’ve been using
- A substitution taper – where, if you’ve been using a short-acting benzo like Xanax, you first switch off to a longer acting benzo like diazepam, and then once stable on the diazepam, start to taper down
The Benefits of a Substitution Taper (to Diazepam)
Many clinicians recommend switching to diazepam prior to initiating a tapering program.
- Diazepam has a very long half-life (between 20 and 100 hours). Because of this, benzo levels in the bloodstream remain very constant and you avoid the peak and valley levels seen with shorter acting benzos like alprazolam. These more constant benzo levels facilitate neural recovery (the brain ‘heals’ faster) and minimize withdrawal symptoms.
- Diazepam has very low tablet strengths, and this low potency allows you to easily make very small dose reductions. For example, It’s quite easy to take one fewer 2mg diazepam per day – it’s much harder to shave 0.1 mgs of Xanax off a 0.5 mg tablet.6
Because of diazepam’s long half-life, and difficulties in finding exact equivalent dosages between benzos, it is generally recommended that you switch over to diazepam gradually, in a step-wise fashion over a period of weeks, and then once stable on diazepam, start your tapering from there.7
Roughly Equivalent Diazepam Dosages
Because of the wide variations in half-life and thus variations in how people respond to different benzodiazepines (influenced by factors such as age and hepatic impairment) it’s quite difficult to provide an exactly equivalent diazepam to other benzodiazepine dosage.
According to the Victorian (Australia) Gov. drug withdrawal practice guidelines, as of 2009, 5 mgs of diazepam was approximately equivalent to:8
- Alprazolam (Xanax, Kalma) 0.5 mg
- Oxazepam (Serepax, Murelax) 30 mg
- Clonazepam (Rivotril) 0.5 mg
- Nitrazepam (Mogadon, Aldorm) 5 mg
- Flunitrazepam (Hypnodorm) 1 mg
- Lorazepam (Ativan) 0.5 mg
So, for example, if you wanted to switch from 2mgs of Xanax to an equivalent amount of diazepam you would need to take 20 mgs of diazepam.
- However, this is just a rough guideline and you won’t necessarily feel exactly the same on a theoreticallyequivalent dosage of a different benzodiazepine.
- So, what you need to do, is transfer gradually off your current benzo to diazepam, and then dial in a minimum dose of diazepam that keeps withdrawal symptoms at bay but doesn’t leave you feeling over sedated. Once stable on this dose, you can start your tapering regimen.
Example Tapering Schedules
- Reduce your dose by 10% every 1 or 2 weeks until you’re at 20% of your original dose, and then taper down by 5% every 2 to 4 weeks9
Or, a more aggressive approach, endorsed by the Oregon State College of Pharmacy10
- Taper by 25% per week for the first 2 weeks and then start a 12.5% reduction per week for the next to 6 weeks (note, tapering usually gets harder as you progress to smaller doses). This aggressive approach may not be suitable for people who have tried and failed in the past with a tapering regimen. For such people a 6 month tapering regimen is recommended.
As a general rule, it doesn’t really matter how slowly you taper and it’s a good idea to stabilize at a dosage before moving further down. Reductions tend to get harder in the second half of the process, so it’s OK to slow down as you need to, as you approach the finish line.
However, you should definitely avoid:
- Taking extra pills in times of great stress
- Going back up to an earlier plateau, if a new dosage seems difficult
- Using other substances that mimic the GABA effects of benzos (this obviously corrupts the tapering process)
Avoiding Alcohol during Benzo Withdrawals
Drinking may worsen your withdrawal symptoms (especially the morning after) but there’s another important reason to avoid alcohol until you feel better.
- You experience withdrawal symptoms because your GABA system is all messed up and it needs to normalize before you’ll feel better
- Alcohol increases GABA activity, just like benzos do
- So if you drink, you slow your brain’s healing and there’s a risk that you’ll just start to drink more and more as you taper further as a way to compensate, without really allowing your brain a chance to heal
And if you do this, at the end of it all not only is your GABA system still out of whack – now you’ve got an alcohol problem too!
Coping with Withdrawal Symptoms: Self Help
To minimize your symptoms:12
- Strive to eat a healthy diet with lots of fresh fruits and vegetables. Drink lots of water
- Avoid caffeine
- Exercise (as much as you can…you can’t do too much)
- Rest up as well as you can
- Keep a recovery diary and chart the progress you make
- Ask for help and support from friends or family for things like household chores and general responsibilities
- If interested, explore alternative healing, such as acupuncture or Chinese medicine11
- Avoid using alcohol or drugs. They may help in the short term but will exacerbate symptoms over the long run
- Avoid making major decisions or adding unnecessary stress to your life while going through withdrawals
- Relax in a hot bath
- Practice relaxation techniques, like deep breathing exercises
- Meditate and practice mindfulness
- Learn Cognitive Behavioral Therapy (CBT) techniques (with a therapist or in a group, or on your own through a self help program or books) and learn to challenge negative thoughts and harmful inaccurate beliefs
Keeping Things in Perspective
Staying focused on how bad you’re feeling won’t help you feel better, and the more you obsess about your symptoms, the worse you’ll perceive those symptoms to be – in fact, sometimes worrying about how you’ll feel after dose reductions causes more negative symptoms than the dose reduction itself!13
One trick you can use to minimize the worry is to accept that after each dose reduction you might catch a touch of ‘Benzo Flu’
Think objectively about how you feel after a dose reduction and compare these symptoms to how you feel when you catch a cold or flu. Are they comparable? When you get a flu do you worry a lot about how terrible you’re feeling or do you just accept that you’ll feel crummy for a few days and that you’ll feel better in time.
With benzo withdrawal symptoms it’s pretty much the same thing. You may feel crummy for a short time after a dose reduction, but you’ll feel better quickly enough, so why not just think of your symptoms as a case of benzo flu – and since you know that this flu will pass quickly enough, you don’t need to get too stressed about how bad you feel.
Should You Consider Counseling?
You should, ideally, seek a doctor’s medical supervision to help you with the withdrawal process, but on top of this, should you also seek out some form of counseling support?
Anxiety is the most commonly experienced benzo withdrawal symptom. This anxiety is temporary and will go away as your body readjusts, but if you find it very uncomfortable you may find counseling helpful.
- A counselor or psychologist can help you learn behavioral and cognitive behavioral techniques to manage anxiety. These techniques can be learned in a handful of sessions and can be practiced and implemented as needed, on your own.
- You may also find a community or online support group helpful. It can be reassuring to hear from others who are going through or have gone through similar experiences.People in support groups, or even within online support forums, can provide helpful information and support.
Basically, this is a tough process, and if you’re having trouble coping with your withdrawal symptoms, it’s entirely reasonable to seek out extra helpful support and advice.
Medications That Can Ease Withdrawal Symptoms
Your doctor may prescribe you medications that can reduce the severity of some withdrawal symptoms. Medications sometimes prescribed include:14
- Propranolol – to help reduce tremor and sweating (for up to about 3 weeks)
- Non-benzodiazepine sedatives like antihistamines or sedative antidepressants – to help reduce insomnia (short duration, about 2 weeks)
- Carbamezepine (and other anticonvulsants) – to reduce the risk of convulsions
Less Common Withdrawal Symptoms
In addition to the more commonly experienced withdrawal symptoms from the list above, some people may experience one or more of the following:15
- Agoraphobia
- Tiredness and lethargy – heavy limbs
- Breathing problems or tightness in chest
- Blurry vision, sore eyes, sensitivity to light or seeing spots
- Becoming very sensitive to sounds, or hearing a ringing in ears
- Dizziness or feeling like the ground is moving
- A lack or co-ordination or balance
- Feeling like things aren’t real (depersonalization)
- Heart palpitations
- Digestive problems, diarrhea, constipation or nausea
- Nightmares
- Headaches or a sense of tightness in the head
- Urinary problems – urgency, incontinence
- Excessive sweating
- Psychotic symptoms (hallucinations)
- Anger or rage
- Changes in libido
- Change in appetite, loss of taste, weight gain or loss
- Menstrual changes
- Difficulty swallowing, soreness in mouth and tongue
- Intrusive thoughts or memories
- Hyperactivity
- Feelings of numbness or pins and needles
- Increased emotional reactivity
- Suicidal thoughts
- Impulsive behaviors
- Many others
Side Effects of Zithromax (z-pack or Azithromycin)
[svpVideo v=1]
[svpVideo v=2]
Possible side effects of Zithromax
Like all medicines, even a single dose of Zithromax can trigger side effects, some of which may include:
- Mucocutaneous effects: allergic skin rash, photosensitivity, pain in the joints, hives, itching, edema and generalized allergic reactions. Rare cases of severe skin reactions have been reported.
- Digestive side effects: nausea, vomiting, indigestion, diarrhea (rarely severe), abdominal pain, pancreatitis (pancreas disease).
- Hepatic effects: increased liver enzymes (reversible when treatment is stopped); severe liver damage in extremely rare cases.
- Neurological effects: dizziness; rare cases of convulsions.
- Blood effects: Isolated cases of abnormally low levels of platelets.
- Psychiatric: rare cases of aggressive behavior, nervousness, restlessness, and anxiety.
- Genital effects: inflammation of the vagina.
- Auditory effects: rare cases of hearing impairment with whistling, ringing in the ears or deafness.
- General effects: fungal infections.
What are possible side effects of Neulasta?
[svpVideo v=1]
What are possible side effects of Neulasta?
Neulasta may cause serious side effects, including:
- Spleen rupture. Your spleen may become enlarged and can rupture. A ruptured spleen can cause death. Call your healthcare provider right away if you have pain in the left upper stomach area or your left shoulder.
- A serious lung problem called Acute Respiratory Distress Syndrome (ARDS). Call your healthcare provider or get emergency care right away if you have shortness of breath with or without a fever, trouble breathing, or a fast rate of breathing.
- Serious allergic reactions. Neulasta can cause serious allergic reactions. These reactions can cause a rash over your whole body, shortness of breath, wheezing, dizziness, swelling around your mouth or eyes, fast heart rate, and sweating. If you have any of these symptoms, stop using Neulasta and call your healthcare provider or get emergency medical help right away.
- Sickle cell crises. You may have a serious sickle cell crisis if you have a sickle cell disorder and receive Neulasta. Serious sickle cell crises have happened in people with sickle cell disorders receiving Neulasta that has sometimes led to death. Call your healthcare provider right away if you have symptoms of sickle cell crisis such as pain or difficulty breathing.
- Kidney injury (glomerulonephritis). Neulasta can cause kidney injury. Call your healthcare provider right away if you develop any of the following symptoms:
- swelling of your face or ankles
- blood in your urine or dark colored urine
- you urinate less than usual
- Capillary Leak Syndrome. Neulasta® can cause fluid to leak from blood vessels into your body’s tissues. This condition is called “Capillary Leak Syndrome” (CLS). CLS can quickly cause you to have symptoms that may become life-threatening.
- Get emergency medical help right away if you develop any of the following symptoms:
- swelling or puffiness and are urinating less often
- trouble breathing
- swelling of your stomach-area (abdomen) and feeling of fullness
- dizziness or feeling faint
- a general feeling of tiredness
– See more at: https://www.neulasta.com/learn-about-neulasta/side-effects/#sthash.kz4NY9jb.dpuf
Increased white blood cell count (leukocytosis). Your healthcare provider will check your blood during treatment with Neulasta.
What is Neulasta?
Neulasta is a man-made form of granulocyte colony-stimulating factor (G-CSF). G-CSF is a substance produced by the body. It stimulates the growth of neutrophils, a type of white blood cell important in the body’s fight against infection. Acute Radiation Syndrome: The effectiveness of Neulasta for this use was only studied in animals, because it could not be studied in people.
Please download the Patient Product Information
Manufacturer Website for Neulasta
Why Don’t You Sell Acidoll?
Mary Asks Dale
Why Don’t You Sell Acidoll?
Dale Answers
To me, the product makes little logic in it combinesBetaine HCL and Pepsin with Pancreatin
Betaine HCL to increase acid in stomach
According to NIH.gov Betaine HCl significantly lowered gastric pH by 4.5 (± 0.5) units from 5.2 (± 0.5) to 0.6 (± 0.2) (P < 0.001) during the 30 min interval after administration. The onset of effect of betaine HCl was rapid, with a mean time to pH < 3 of 6.3 (± 4.3) min. The reacidification period was temporary with a gastric pH < 3 and < 4 lasting 73 (± 33) and 77 (± 30) min, respectively. Betaine HCl was well tolerated by all subjects. In healthy volunteers with pharmacologically induced hypochlorhydria, betaine HCl was effective at temporarily lowering gastric pH.
Pepsin is a PH of 1.5 – 1.6 and works in the stomach
And Pancreatin with is a BASE (alkaline) with a pH 9.0 (Google it) and is never naturally present in the stomach It is delivered into the small intestine after the stomach is done breaking down the food particles and along with the other fluids issued when the stomach squirts the liquid food (Chime) has to neutralize the acid because after the stomach the balance of the transit of nutrient and waste has to be a bit alkaline.
I recommend pancreatic enzymes be consumed thirty minutes prior to food in order or them to pass peacefully through the stomach leading in the small intestine and be ready for the food after the stomach is done with its job.
So Below are the two products to consume
To increase stomach acid
In increase Pancreatin in small intestine
Pancreatic Enzyme Capsules or Tablets? What is Best For You?
How to calculate needed enzymes
Pancreatin, 1200 mg, 1,000 Capsules, Take 30 Minutes Before Food
Pancreatic Enzyme Capsules or Tablets? What is Best For You?
We now have available Pancreatic Enzymes (USP) in both Capsules and Tablets.
Advantages of Tablets:
- Better at surviving stomach acid (for people unable to consume the enzymes well ahead of the meal – and for snackers too)
- More rugged for carrying around in pocket or purse (in ziplock baggies)
Disadvantages of Tablets:
- The fillers and binders can be offensive to some sensitive people
Advantages of Capsules:
- Sensitive people prefer capsules generally due to the reduction or elimination of fillers and binders
- Many people find capsules easier to swallow
Disadvantages of Capsules:
- The timing of the consumption of the enzymes in capsules is much more critical than in tablets. Pancreatic enzymes are alkaline and without the binders and fillers found in the tablets they can (when you fail to consume them thirty minutes or more prior to eating) reduce the stomach acid and therefore make the stomach less successful in doing it’s job of chemically breaking down food prior to it’s delivery to the small intestine (where the enzymes complete the process of liberating the nutrition that is held within the food).
- Capsules are more fragile than tablets and prone to breaking when carried in a ziplock baggie. It is important to understand that you should not chew up a pancreatic capsule or open it and add it to anything because it is quite caustic and can cause discomfort to eyes, nose, mouth or any mucous area.
[table id=15 /]
Oxycodone
This drug is a highly addictive semisynthetic opioid. By modifying a plant-based drug used for centuries,
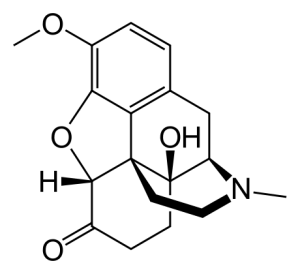
Oxycodone the pharmaceutical industry has been able to create a substance many times as addictive as the original formula. If you are currently taking this drug you will be facing a challenge to get off it.
You can manage pain with coffee enemas (up to five per day) as you reduce very gradually the drugs.
Oxycodone is a semisynthetic opioid synthesized from thebaine, an opioid alkaloid found in the Persian poppy, and one of the many alkaloids found in the opium poppy. It is a moderately potent opioid analgesic, generally indicated for relief of moderate to severe pain. Oxycodone was developed in 1917 in Germany] as one of several semi-synthetic opioids in an attempt to improve on the existing opioids.
Oxycodone is available as single-ingredient medication in immediate release and controlled release.
Interactions
Oxycodone is metabolized by the enzymes CYP3A4 and CYP2D6, and its clearance therefore can be altered by inhibitors and inducers of these enzymes.[26] Natural genetic variation in these enzymes can also influence the clearance of oxycodone, which may be related to the wide inter-individual variability in its half-life and potency.[26]
Ritonavir or lopinavir/ritonavir greatly increase plasma concentrations of oxycodone in healthy human volunteers due to inhibition of CYP3A4 and CYP2D6. Rifampicin greatly reduces plasma concentrations of oxycodone due to strong induction of CYP3A4. There is also a case report of fosphenytoin, a CYP3A4 inducer, dramatically reducing the analgesic effects of oxycodone in a chronic pain patient. Dosage or medication adjustments may be necessary in each case.]
(For lists of CYP3A4 and CYP2D6 inhibitors and inducers, see here and here, respectively.)
Link over to Wikipedia for a big document on the drug
Side Effects
Major Side Effects
If any of the following side effects occur while taking oxycodone, check with your doctor immediately:Less common:
- Chills
- cold sweats
- confusion
- difficult or labored breathing
- dizziness, faintness, or lightheadedness when getting up suddenly from a lying or sitting position
- fever
- tightness in the chest
- twitching
- RareAbdominal or stomach pain
- bloating or swelling of the face, arms, hands, lower legs, or feet
- blood in the urine
- burning while urinating burning, crawling, itching, numbness, prickling, “pins and needles”, or tingling feelings
- feelings
- chest pain
- convulsions
- cough
- decrease in the frequency of urination
- decrease in urine volume
- decreased urine output
- difficult or painful urination
- difficulty in passing urine (dribbling)
- difficulty with swallowing
- dizziness
- dry mouth
- fainting
- fast, irregular, pounding, or racing heartbeat or pulse
- feeling of warmth or heat
- flushing or redness of the skin, especially on the face and neck
- frequent urination
- headache
- hives, itching, or skin rash
- increase in heart rate
- increased thirst
- increased volume of pale, dilute urine
- lightheadedness
- muscle pain or cramps
- nausea or vomiting
- puffiness or swelling of the eyelids or around the eyes, face, lips, or tongue
- rapid breathing
- rapid weight gain
- severe constipation
- severe vomiting
- shakiness in the legs, arms, hands, or feet
- sunken eyes
- sweating
- swelling or puffiness of the face
- swollen, painful, or tender lymph glands in the neck, armpit, or groin
- thirst
- tingling of the hands or feet
- trembling or shaking of the hands or feet
- unusual tiredness or weakness
- unusual weight gain or loss
- wrinkled skin
Incidence not known:
- Blurred vision
- choking
- clay-colored stools
- cold, clammy skin
- dark urine
- diarrhea
- fast, weak pulse
- gagging
- irregular, fast, slow, or shallow breathing
- loss of appetite
- pale or blue lips, fingernails, or skin
- unconsciousness
- unpleasant breath odor
- very slow heartbeat
- yellow eyes or skin
If any of the following symptoms of overdose occur while taking oxycodone, get emergency help immediately:
Symptoms of overdose:
- Change in consciousness
- chest pain or discomfort
- constricted, pinpoint, or small pupils (black part of the eye)
- decreased awareness or responsiveness
- extreme drowsiness
- loss of consciousness
- no muscle tone or movement
- severe sleepiness
- slow or irregular heartbeat
Minor Side Effects
Some oxycodone side effects may not need any medical attention. As your body gets used to the medicine these side effects may disappear. Your health care professional may be able to help you prevent or reduce these side effects, but do check with them if any of the following side effects continue, or if you are concerned about them:
these side effects may disappear. Your health care professional may be able to help you prevent or reduce
these side effects, but do check with them if any of the following side effects continue, or if you are concerned about them:
More common: Difficulty having a bowel movement (stool)
Difficulty having a bowel movement (stool)
drowsiness
lack or loss of strength
relaxed and calm feeling
sleepiness or unusual drowsiness
Less common:
- Abnormal dreams
- acid or sour stomach
- anxiety
- belching
- burning feeling in the chest or stomach
- false or unusual sense of well-being
- heartburn
- hiccups
- indigestion
- stomach discomfort, upset, or pain
- tenderness in the stomach area
- trouble sleeping
- weight loss
- RareAbsent, missed, or irregular menstrual periods
- bad, unusual or unpleasant (after) taste
- bloated or full feeling
- body aches or pain
- change in taste
- change in walking and balance
- changes in vision
- clumsiness or unsteadiness
- congestion
- continuous ringing or buzzing or other unexplained noise in the ears
- crying
- decreased interest in sexual intercourse
- dental caries or tooth decay
- depersonalization
- depression
- difficulty with speaking
- dry skin
dryness or soreness of the throat - excess air or gas in the stomach or intestines
- excessive muscle tone
- feeling of constant movement of self or surroundings
- feeling of unreality
- general feeling of discomfort or illness
- headache, severe and throbbing
- hearing loss
- hoarseness
- hyperventilation
- inability to have or keep an erection
- increase in body movements
- increased appetite
- increased cough
- irritability
- loss in sexual ability, desire, drive, or performance
- loss of heat from the body
- loss of memory
- loss of strength or energy
- muscle pain or weakness
- muscle stiffness
- muscle tension or tightness
- neck pain
- paranoia
- passing of gas
- problems with memory
- quick to react or overreact emotionally
- rapidly changing moods
- red, swollen skin
- restlessness
- runny nose
- scaly skin
- sensation of spinning
- sense of detachment from self or body
- severe sleepiness
- stomach pain, fullness, or discomfort
- swelling or inflammation of the mouth
- tender, swollen glands in the neck
- unusual weak feeling
- voice changes
Furosemide Side Effects
Call your doctor right away if you notice any of these side effects:
Allergic reaction: Itching or hives, swelling in your face or hands, swelling or tingling in your mouth or throat, chest tightness, trouble breathing
Blistering, peeling, red skin rash
Chest pain, shortness of breath
Confusion, weakness, muscle twitching
Dry mouth, increased thirst, muscle cramps, nausea or vomiting, uneven heartbeat
Sudden and severe stomach pain, nausea, vomiting, fever, lightheadedness
Hearing loss, ringing in the ears
Lightheadedness, dizziness, fainting
Severe diarrhea
Unusual bleeding or bruising
Yellow skin or eyes
If you notice these less serious side effects, talk with your doctor:
Loss of appetite, stomach cramps
If you notice other side effects that you think are caused by this medicine, tell your doctor.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
Side Effects of This Medicine
Along with its needed effects, a medicine may cause some unwanted effects. Although not all of these side effects may occur, if they do occur they may need medical attention.
Check with your doctor immediately if any of the following side effects occur:
Rare
Incidence not known
-
Back or leg pains
-
black, tarry stools
-
bleeding gums
-
blistering, peeling, or loosening of the skin
-
bloating
-
blurred vision
-
burning, crawling, itching, numbness, prickling, “pins and needles”, or tingling feelings
-
changes in skin color, pain, tenderness, or swelling of the foot or leg
-
clay-colored stools
-
cloudy urine
-
cold sweats
-
confusion
-
continuing ringing or buzzing or other unexplained noise in the ears
-
cracks in the skin
-
darkened urine
-
difficulty breathing
-
dizziness, faintness, or lightheadedness when getting up from a lying or sitting position
-
dry mouth
-
fast heartbeat
-
flushed, dry skin
-
fruit-like breath odor
-
greatly decreased frequency of urination or amount ofurine
-
hearing loss
-
increased hunger
-
increased thirst
-
indigestion
-
itching
-
loss of appetite
-
nosebleeds
-
pale skin
-
pinpoint red spots on the skin
-
red, irritated eyes
-
red, swollen skin
-
spots on your skin resembling a blister or pimple
-
sweating
-
swelling of the feet or lower legs
-
trouble breathing with exertion
-
unusual weight loss
-
yellow eyes or skin
Get emergency help immediately if any of the following symptoms of overdose occur:
Symptoms of overdose
-
Decreased urination
-
drowsiness
-
increase in heart rate
-
irritability
-
mood changes
-
numbness, tingling, pain, or weakness in the hands, feet, or lips
Some side effects may occur that usually do not need medical attention. These side effects may go away during treatment as your body adjusts to the medicine. Also, your health care professional may be able to tell you about ways to prevent or reduce some of these side effects. Check with your health care professional if any of the following side effects continue or are bothersome or if you have any questions about them:
Incidence not known
-
Feeling of constant movement of self or surroundings
-
hives or welts
-
increased sensitivity of the skin to sunlight
-
redness or other discoloration of the skin
-
restlessness
-
sensation of spinning
-
severe sunburn
-
weakness
Other side effects not listed may also occur in some patients. If you notice any other effects, check with your healthcare professional.
-
Flonase Side Effects
Flonase (fluticasone) is a synthetic steroid of the glucocorticoid family of drugs and is prescribed for the control of symptoms of allergic and non-allergic rhinitis. Flonase is available as a generic drug, and dosing is usually administered as two sprays in each nostril once daily, or one spray in each nostril twice daily.
The most common side effects of Flonase (fluticasone) include:
- headache,
- back pain,
- sore throat,
- sneezing,
- cough,
- nausea,
- vomiting,
- menstrual problems,
- loss of interest in sex,
- nosebleeds,
- sinus pain, and
- sores or white patches inside mouth or around your nose.
Flonase has also been associated with hypersensitivity reactions (for example, skin rash, itching, facial swelling, and anaphylaxis).
The recommended starting dosage of Flonase in adults is 2 sprays (50 mcg of fluticasone propionate each) in each nostril once daily (total daily dose, 200 mcg). Drug interactions and warnings include Norvir (ritonavir) and Nizoral (ketoconazole). Taking either one of these drugs with Flonase may increase the blood concentrations of Flonase and potentially increase its side effects. Flonase should only be used during pregnancy when it is absolutely necessary. There have not been adequate studies of Flonase and concentrations in breast milk; therefore, Flonase should be avoided while breastfeeding unless it is absolutely necessary.
Our Flonase Side Effects Drug Center provides a comprehensive view of available drug information on the potential side effects when taking this medication.
FLONASE® Allergy Relief is meant to work in your nose. Never use in your eyes or mouth.
If you or your child have an allergic reaction to this product, with sudden swelling of the face or tongue, a rash, or wheezing or feeling faint, stop using FLONASE® Allergy Relief and see a doctor right away.
If you or your child experiences a nose injury with severe or frequent nosebleeds, apply pressure to your nose. Stop using FLONASE® Allergy Relief and see a doctor right away.
If you or your child experiences a constant whistling sound that does not go away, this could be a sign of damage to your nose. Stop using FLONASE® Allergy Relief and see a doctor right away.
If you or your child experiences cloudy or reduced vision, it could be the result of eye conditions such as cataracts or glaucoma. Be sure to schedule a yearly eye exam to check for these conditions.
If administering to your child, talk to their pediatrician if you are concerned they may experience certain growth effects, such as a slower growth rate as a result of using FLONASE® Allergy Relief. Also, speak to your doctor if your child is between the ages of 4 and 11 needs to use FLONASE® Allergy Relief for longer than 2 months a year.
Talk to your doctor or pharmacist if you or your child experiences other side effects such as headaches or sneezing, a bad taste or smell, minor nosebleeds, or a dry or irritated nose or throat.
Finally, please read the Drug Facts on the back of the FLONASE® Allergy Relief or package to be aware of any additional information that may be helpful to you. If you have any concerns about side effects, talk to your doctor.
Use as directed. Please see specific products for full labeling information.
May Be Addicted To Morphine?
Morphine is an extremely addictive painkiller. In fact, morphine addictive properties make it a Schedule II narcotic under the Controlled Substances Act. When addicts try to quit morphine, they often experience severe cramps, pains and anxiety which can result in using the drug again in order to avoid withdrawal. But what are some clear signs of morphine addiction?
Here, we will explore the signs and symptoms of morphine addiction and let you know what you can do to help someone who is addicted. Then, we invite your questions about treating morphine addiction in the comments section at the end.
Symptoms Of Morphine Addiction
Morphine addiction can start as a prescribed medication to solve real pain issues. However, having morphine in the system can lead to habitual drug seeking or using morphine other than intended. Many users find that they cannot stop after even a few weeks of regular dosing.
Morphine addiction can result in a range of symptoms from weight loss to vomiting and memory problems. There are also obvious emotional signs of morphine addiction which can include anxiety, hallucinations, depression and irritability. Morphine addiction also reduces the addict’s level of consciousness, which affects their ability to be fully aware of their surroundings.
In addition to morphine withdrawal symptoms after a missed dose (lack of appetite, irritability, weight loss, drowsiness and sweating), Diagnostic and Statistical Manual of Mental Disorders clinical criteria for morphine addiction include:
- A strong desire to take morphine
- Difficulties controlling morphine use
- Entering a psychological withdrawal state when the drug use is stopped
- Increased doses due to tolerance
- Neglect of alternative interests because of morphine use
- Persistent morphine use despite harmful consequences physically or mentally
Morphine Addiction Symptoms: Can They Be Treated?
I recomend gradual reduction with many coffee enemas, below ar the standard methods.
Morphine addiction symptoms can be treated through several different types of therapies and/or the use of prescription medications.
Psychological treatments – Psychotherapy and behavioral therapy are two of the most successful interventions for morphine addiction. These treatments address the emotional and cognitive aspects of addiction to resolve and change past behaviors.
Opiate replacement therapy – Replacement therapy attempts to curb addiction to morphine by replacing morphine with a less euphoric opioid, such as methadone or buprenorphine, which is taken under medical supervision. Replacement therapy helps addicts to lead a normal life while being treated with a substance that stops them from experiencing the harsh morphine withdrawal symptoms and cravings.
Prescription medications – There are medications available for morphine addiction and when used in combination with behavioral treatment programs increase chances of quitting morphine significantly. Prescription medications include anti-anxiety meds, antidepressants, and drugs such as nalexone or buprenorphine used to address withdrawal symptoms. Patients are less likely to become dependent on buprenorphine and when they stop the withdrawal symptoms are much weaker.
Morphine addiction support groups – Morphine addiction support groups can be useful for helping treat morphine addiction symptoms. Many addicts can find a sense of community by joining a support group and get further assistance psychologically months down the road to help prevent relapse. Support groups can be found at your local rehab center.
